Keywords: OSA, CPAP, APAP, EPR, C-Flex, A-Flex, pressure support, pressure sensitivity, air hunger, AHI, residual AHI, therapeutic efficacy, comfort settings.
The intended audience for this post includes (1) individuals who use CPAP and want to know how pressure relief features work, (2) healthcare team members interested in improving their patients' experiences with CPAP therapy.
This content is not medical advice.
Mr. R is a 42-year-old with newly diagnosed obstructive sleep apnea (OSA) on home sleep testing. He opts for treatment with auto adjusting CPAP (4-20 cwp) and foregoes spending any time in the sleep lab.
After figuring out he needs a mask with mouth coverage, he is disappointed in his high apnea hypopnea index (AHI) and lack of symptom improvement. Setting changes have addressed his air hunger (feeling like he needs more air) and pressure intolerance (feeling like he is getting too much air).
Now Mr. R’s machine is set with a pressure range of 6 to 10 centimeters of water pressure (cwp). His AHI is hanging around 8 (we want it <5 if we can manage) and his pressure is consistently hitting 9.8 to 10 cwp. For comfort, the EPR (expiratory pressure relief) is at 3.
I can guess what you may be thinking, because I was thinking it too. The machine probably isn’t set to give enough air to keep his airway open. If his airway isn’t staying open like it should, we have an adequate explanation for his lack of symptom improvement.
There’s something under recognized going on here. Something that you won’t see on a download unless you understand the backstory on “comfort” settings.
“Comfort” Settings: The Backstory
When I trained with my board-certified sleep medicine mentor over a decade ago, the prevailing thought on EPR (™ ResMed) and C-Flex/A-Flex (™ Respironics) settings was that they were comfort features and should not interfere with the effectiveness of therapeutic pressure delivery. These optional settings back off pressure delivery during exhalation in 1 cwp increments, with a maximum differential of 3 cwp. These features were also marketed as a tool to help patients do better with their therapy by making it easier to tolerate. It seemed a reasonable idea, but there were no well-publicized studies on it at the time.
CPAP vs BPAP
People often ask me how CPAP and BPAP are different and why that difference is important?
CPAP (continuous positive airway pressure) delivers one level of air breathing in and the same level breathing out. BPAP (bi-level positive airway pressure) is one level of air breathing in and much less breathing out. For a machine to function as a BPAP, the difference between breathing in pressure (IPAP, inspiratory positive airway pressure) needs to be at least 4 cwp higher than breathing out pressure (EPAP, expiratory positive airway pressure). This difference is called pressure support.
In some cases, I have seen pressure support as high as 10 or 12 cwp. When it is this high, we are trying to ventilate a patient with lung disease of some sort (ie- help air flow in and out of the lungs) rather than simply keep their airway open, which is the primary goal in obstructive sleep apnea (OSA) management with CPAP.
CPAP and EPAP serve the same function. They both keep the airway open. If a BPAP patient needs a pressure bump because their AHI is unacceptably high due to obstructive respiratory events, the EPAP would be the thing to bump, not the IPAP. In CPAP, there’s only one setting to bump: the CPAP pressure setting.
Maximizing “Comfort”
Maxing out the EPR/FLEX setting to 3 on a CPAP machine transitions therapy so it resembles BPAP more closely than CPAP, with a pressure support of 3 cwp. In theory, it may save the patient from having to go with a BPAP machine for pressure intolerance because both modalities are supposed to make it easier for the patient to breathe out.
There are some problems with this. Let’s go back to Mr. R.
We have a pretty good idea he needs more air to keep his airway open. With his EPR set at 3, a pressure range of 6 to 10 cwp, and an average pressure of 9.8-10 cwp, what pressure of air is available to keep his airway open?
Here’s a hint. It’s none of the numbers I have just provided to you.
The pressure keeping his airway open is only going to be 6.8 to 7 cwp because 10 minus 3 equals 7 cwp.
Well, damn.
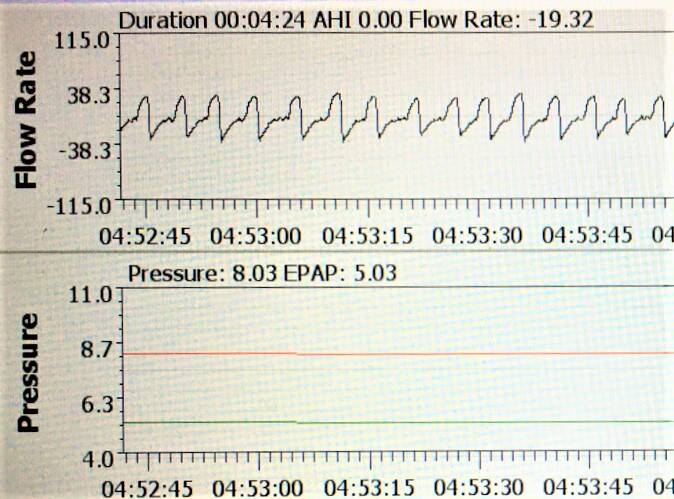
Oscar software print out from a CPAP machine set with EPR of 3.
When a CPAP machine has comfort settings maxed out, the manufacturer-based download software and the machine are reporting the breathing in pressure, not the one keeping the airway open. There is no option in the manufacturer’s software to report two numbers. Perhaps because it wasn’t supposed to make that much of a difference. Or, maybe because it’s only available on models that are bilevel-capable.
And just like that, we’ve identified some uncomfortable facts about CPAP comfort settings.
Some uncomfortable facts about CPAP "comfort" settings
The air pressure reported on the machine download will usually be inaccurate when comfort settings are active. When the contribution of comfort settings gets overlooked, and remains uncompensated for, it has the potential to negatively affect therapeutic outcomes, contributing to failure rather than success. The degree of inaccuracy and how much it can impact therapy depends on:
- The comfort setting itself: EPR/Flex 1, 2, 3, 3+
- The mode: continuous or adjusting
- The pressure setting (or range of settings, if in adjusting mode), and
- Whether or not the patient had a titration sleep study with the comfort setting active.
The higher the “comfort” level, the greater the expected inaccuracy of reported pressure settings, up to 3 cwp.
If the patient had a titration sleep study with maximum comfort settings applied, the differences in pressure to keep the airway open would have already been observed in the lab. We would know, based on lab monitoring, which settings helped, and which ones didn’t. (At least, that's the idea, anyway.) The sleep test reports that come across my desk always have this information readily available, though it may be buried in the technician’s notes.
If comfort settings are applied after the fact, or with an empiric therapy trial the difference in pressure delivery needs to be accounted for.
Side note: An “empiric therapy trial” means no sleep study, just general starting settings in adjusting CPAP mode. The usual manufacturer default is 4 to 20 cwp in adjusting mode, though my sleep doc mentor always preferred 5 to 20 cwp.
A fixed pressure which had been tightly titrated with no or little comfort settings or a tighter adjusting pressure range (i.e.- 5 to 10 cwp) could limit the pressure and impede therapy, whereas a wider one (5 to 20 cwp) is less likely to have this problem (but does have other potential drawbacks).
The Analogy
While the deflation of therapeutic pressure with comfort settings may seem like a confusing concept, I like to think of it like traveling to different time zones. New York is an hour ahead of Texas and three hours ahead of California. Let’s say you’re a New Yorker and you flew to Texas and didn’t change your watch to match, it wouldn’t be that big of deal, because it’s only an hour off. This is similar to a comfort level of 1. You’ll probably wake up an hour earlier and get hungry for dinner an hour earlier, but it’s still in the ballpark with everyone else.
Now, let’s say you flew from New York to California and didn’t change your watch to match. This is like a comfort level of 3. If you didn’t know that 6 am EST is the same as 3 am PST, you’re going to be ready for breakfast before the chickens wake up. You’ll wonder why it stays dark so late into the morning and why everyone around you is just getting dinner on the table when you are ready for bed.
Your watch is still correct in New York, because the time in New York doesn’t change based on where you are, but that’s not what time it is where you find yourself now. The greater the difference, the more disruptive it can be.

Photo credit: Mantas Hesthaven on Unsplash
Case Conclusion
Knowing all of this in light of Mr. R’s struggles, some setting changes were in order. His EPR was changed to 1 and his pressure range was bumped 7 to 11 cwp.
Download data for the most recent 7 days showed an average pressure of 10.8. Breathing out he would be getting 9.8 cwp. His starting pressure would be 6 cwp breathing out and 7 cwp breathing in, rather than 6 cwp breathing in and 4 cwp* breathing out. The AHI went down to 1.9.
* In the preceding example you may have noticed a math error because 6 - 3 = 3. However, 4 cwp is as low as the pressure will go because it can go no lower than the lowest setting available on the machine.
The best part of Mr R’s story is that once his AHI went below 5 and he was getting 5-8 hours of use/night, he felt better. He wasn’t perfect, but he no longer contemplated giving up on his CPAP or labeling it a “worthless piece of junk.”
Pearls for healthcare providers
Resist the urge to set EPR/Flex of 3 indiscriminately. If my patient came from the sleep lab having been titrated using a high comfort setting as part of their final pressure recommendation, I'd feel more reassured at its adequacy. Otherwise script it to patient comfort/preference and beware of how the therapeutic numbers will be altered as this may (or may not) be clinically significant.
Side note: Some sleep physicians consistently recommend which comfort setting to start with based on expertise and sleep lab data; others do not.
If the AHI is not at goal or the patient is struggling with air hunger, make sure it’s not comfort setting interference. A comfort setting of 1 or 2 is less likely to mess with the patient’s therapeutic experience to a clinically significant degree than 3.
Comfort settings will have no activity, regardless of setting, at 4 cwp because the machine will not allow the pressure to go below this basement setting. The most it can go down at 5 cwp is 1 cwp and the most at 6 cwp is 2 cwp. If the floor (lower pressure limit or fixed pressure) is set higher than the basement of 4 cwp, the pressure to keep the airway open will go below the prescribed floor with comfort settings active, but not below the basement.
Pearls for patients
Comfort settings can make a world of difference in a person’s CPAP experience. Some people would have given up on therapy ages ago without them. Comfort settings are not universally benign. If you are struggling with your therapy, it’s a good idea to bring up your concerns to your healthcare team (because this is not intended as medical advice). If your EPR/Flex is maxed out at 3, keep in mind that it could be contributing to difficulties under limited circumstances. Your management team should be able to help sort it out.
Not all healthcare providers who manage CPAP have comfort settings on their radar as a possible pain point. The data is not reported intuitively on manufacturer's download software, so it's an easy input to overlook. The prevailing mindset, even among many highly specialized, respected physicians used to be that these settings were of little technical consequence. While that remains a mostly true statement, today's case example highlights a scenario where backing off a comfort setting (in addition to other setting changes) made a difference for the better in a person's experience with CPAP.
Today's reference
If you want to read peer-reviewed research on this subject from The Journal of Clinical Sleep Medicine, here’s the link to a research paper published 2016 which backs up what I have tried to explain here. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4773618/#__ffn_sectitle
Test your knowledge:
With a comfort setting of 3 and a fixed pressure of 7 cwp, a CPAP user feels more comfortable than with comfort settings off and a fixed pressure of 5 cwp.
Which of these two settings are providing more air to keep the airway open?
Why does one pressure feel better than the other?
For more information and resources on sleep apnea management, sign up for my email list on my website, www.TheSleepNP.com, or send an email to info@thesleepnp.com.
To get periodic content updates, follow The Sleep NP on social media: Facebook, YouTube, and LinkedIn. When you like, follow, and subscribe, you’ll get updates as I post them.
If you like what you’re seeing from the Sleep NP, please share it. There are so many people suffering with sleep apnea and struggling with their CPAP therapy. While this content is not formal medical advice (and does not replace a patient’s healthcare team), you’ll be assisting me with my goal of helping more people sleep better so they can feel better and do better.
Thank you in advance.
Add comment
Comments
Uncomfortable facts about CPAP comfort setting was shared in our CPAP group and was most instructive. Thanks